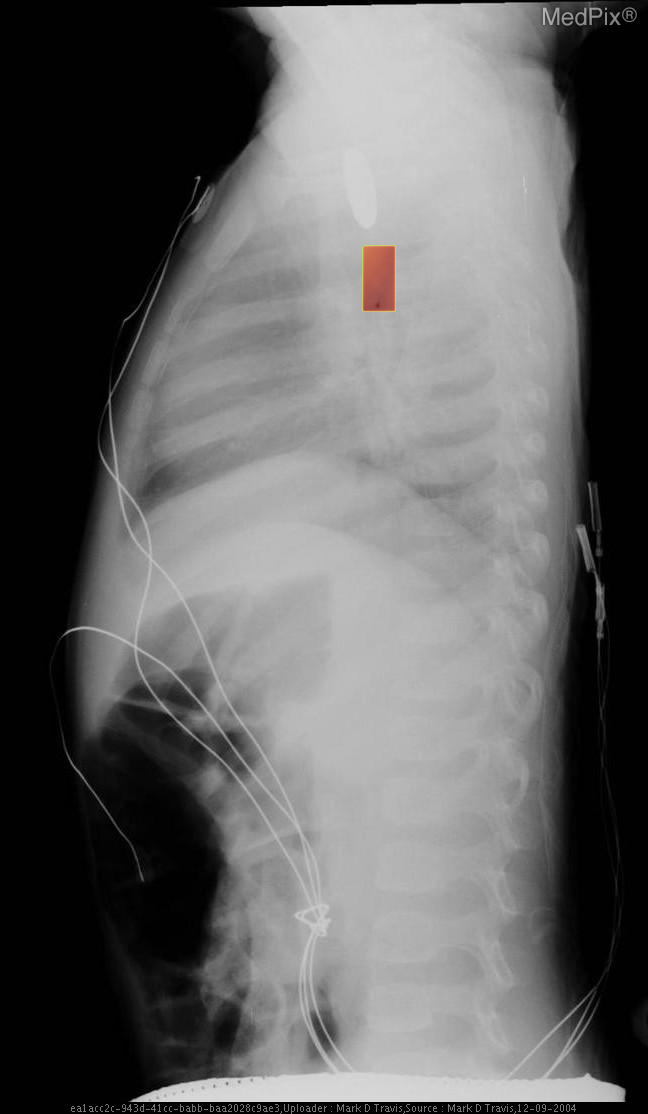
Esophageal foreign body - Coin ingestion


- Age: 1
- Sex: Male
- Modality: X-ray
- Region: Chest
- Country: N/A
- State: N/A
- City: N/A
- Diagnosis: Esophageal foreign body
🧠 AI Suggestion
- Frontal chest X-ray in a pediatric patient shows a round, well-defined radiopaque object projected over the upper thoracic region, likely within the midline.
- The object is seen in the region posterior to the trachea and anterior to the vertebral column, consistent with the expected course of the esophagus.
- No evidence of double halo or step-off suggesting a button battery (appears uniform in density).
- The cardiac silhouette and diaphragm contours are within normal limits.
- Lungs are clear without focal consolidation, pneumothorax, or effusion.
- Bony structures appear intact, no acute fractures noted.
- No subcutaneous emphysema or soft tissue gas.
- Several monitoring leads and lines seen externally, no invasive lines visualized.
2) Most likely diagnosis and why:
Esophageal foreign body (radiopaque coin) in the upper thoracic esophagus. The central, midline location on this frontal image and the uniform circular density without polarity markers (seen in coins rather than button batteries) strongly suggest a coin lodged in the esophagus rather than the trachea (which typically lies anteriorly and shows overlapping on lateral projection). Context consistency: Consistent, as the provided context describes coin ingestion in a 1-year-old male. Confidence: 95%
3) Next best diagnostic step:
Obtain a lateral chest X-ray to confirm the object's placement within the esophagus versus the trachea. The lateral projection will demonstrate whether the object lies posterior (esophagus) or anterior (trachea). Prompt clinical correlation with symptoms of airway compromise should be performed before further imaging if respiratory distress is present.
4) Key differential or confirmatory test:
The main differential is a tracheal foreign body. The lateral X-ray will help distinguish the location. If uncertainty persists or complications are suspected (e.g., perforation or migration), a contrast esophagram or endoscopic evaluation may be necessary for definitive localization and retrieval planning.
5) Possible treatment or management:
Urgent endoscopic removal under airway-protected anesthesia** is indicated for esophageal foreign bodies in children, especially if in the upper esophagus, to prevent mucosal injury or aspiration. If symptomatic with airway obstruction, emergent removal is required. Post-extraction, inspect for mucosal injury or perforation and monitor for stricture development.
📑 Guidelines Summary (uploaded diagnosis) — Esophageal foreign body
Evaluation of nontraumatic chest wall pain focuses on distinguishing musculoskeletal from serious cardiopulmonary or neoplastic causes and guiding targeted imaging choices.
- No imaging if localized pain clearly musculoskeletal and no systemic or cardiopulmonary red flags.
- Radiography chest recommended first-line for unclear etiology, risk factors, or persistent symptoms.
- CT chest with contrast for suspected chest wall mass, fracture, infection, or tumor invasion.
- Non-contrast CT when bony pathology suspected and vascular lesion not a concern.
- MRI chest when soft tissue, marrow, or nerve involvement suspected or CT inconclusive.
- Ultrasound useful for superficial masses, abscess, or muscle strain; dynamic evaluation possible.
- Red flags: history of malignancy, infection signs, systemic symptoms, hemoptysis, unexplained weight loss.
- Avoid unnecessary imaging in reproducible musculoskeletal pain that improves with palpation or movement.
- Follow-up imaging guided by clinical change, non-resolving symptoms, or abnormal prior findings.
- Pitfalls include mistaking referred pain (cardiac, pulmonary, gastrointestinal) for chest wall origin.
- Timely cross-sectional imaging when initial studies negative but clinical suspicion for deeper disease remains.
🤖 Guidelines Summary (AI diagnosis) — Routine Chest Imaging
Routine chest imaging decisions hinge on clinical indication, risk factors, and prior imaging to minimize unnecessary radiation and optimize diagnostic yield.
- Asymptomatic adults without risk factors generally should not undergo routine chest radiography or CT.
- Pre-employment or screening chest radiographs are not indicated in healthy individuals with normal examination.
- Initial chest X-ray is appropriate for new cardiopulmonary symptoms such as cough, fever, dyspnea, or chest pain.
- Low-dose CT is first-line for lung cancer screening in high-risk smokers meeting guideline criteria.
- Repeat chest imaging is unnecessary if prior films within 6 months show stability and no new symptoms arise.
- CT chest without contrast is preferred for evaluating pulmonary nodules or interstitial lung disease.
- CT angiography is reserved for suspected pulmonary embolism or vascular abnormality based on clinical risk scores.
- Do not perform follow-up imaging for acute pneumonia if symptoms resolve and risk factors are absent.
- Red flags warrant imaging: hemoptysis, unexplained weight loss, persistent dyspnea, or severe pleuritic pain.
- Pitfalls include overuse of CT for mild respiratory complaints and failure to compare with prior studies.
Comments
No comments yet.
Please log in to comment