Meningioma
Low confidence
High confidence
- Age: 38
- Sex: Female
- Modality: MRI
- Region: Brain
- Country: N/A
- State: N/A
- City: N/A
- Diagnosis: Meningioma
🧠 AI Suggestion
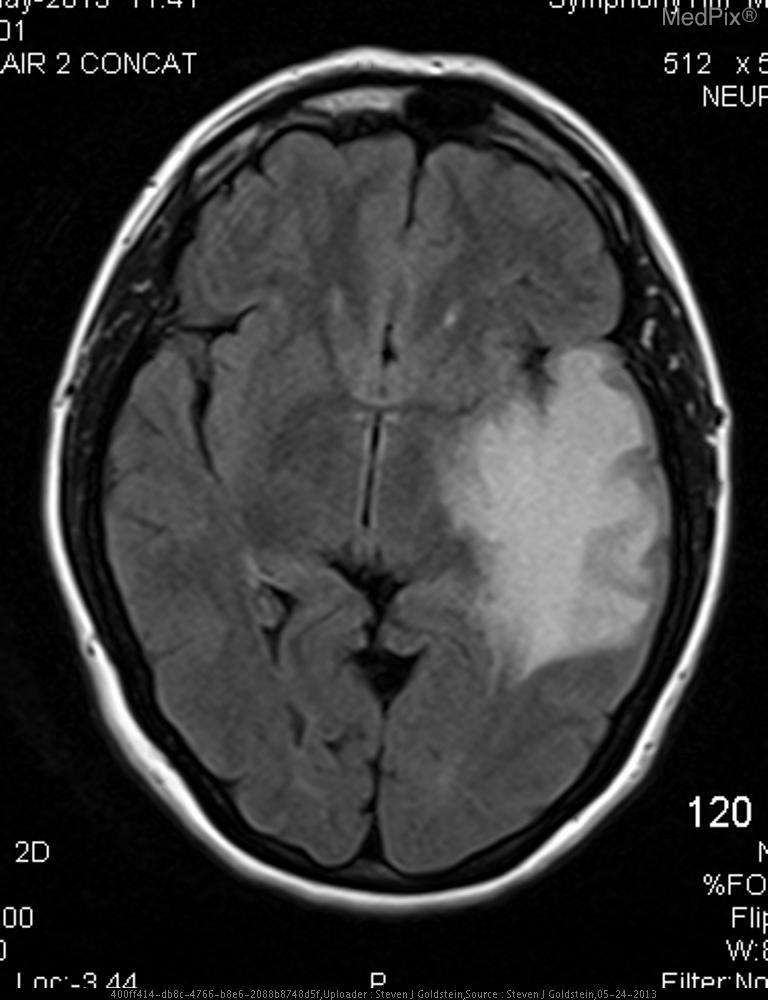
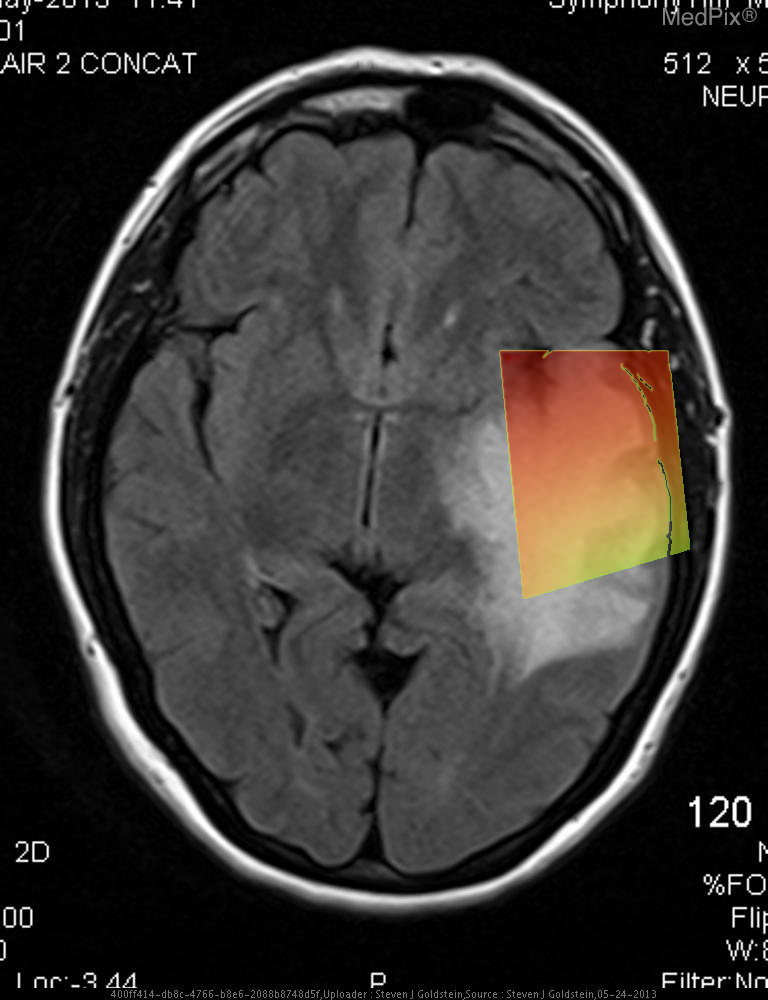
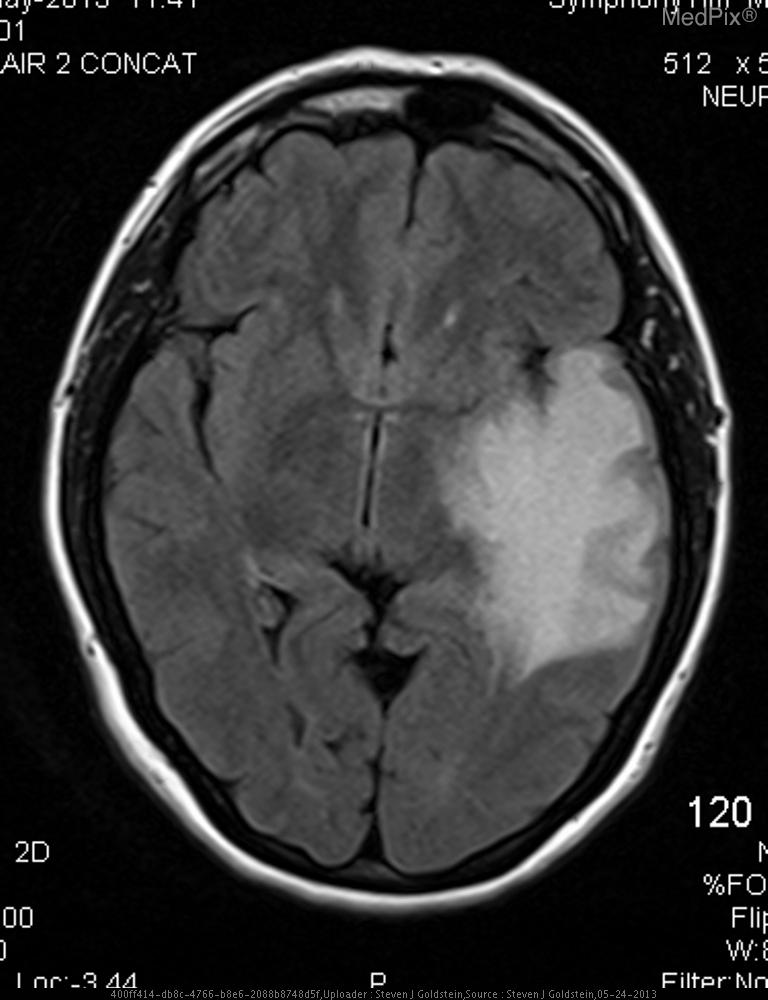
1) Findings:
- A well-defined, extra-axial, dural-based mass is visible over the image-right (patient-left) frontoparietal convexity region.
- The lesion shows heterogeneously hyperintense signal intensity on this FLAIR MRI sequence.
- There is adjacent cortical sulcal effacement and underlying vasogenic edema extending into the adjacent white matter.
- Associated mild local mass effect with rightward (image-left, patient-right) midline shift is evident.
- The lesion margin appears broad-based against the inner table of the skull, with subtle dural thickening (“dural tail” sign possible).
- No hemorrhagic or cystic necrosis component clearly noted on this single sequence.
- Ventricles appear compressed on the image-right (patient-left) side due to mass effect.
- Cortical gray–white differentiation otherwise preserved outside the area of edema.
2) Most likely diagnosis and why:
Extra-axial dural-based mass consistent with meningioma. The smooth, broad-based extra-axial location, dural attachment, and presence of vasogenic edema with mass effect are characteristic features of a meningioma. The rounded contour and preservation of cortical gray–white matter interface favor a meningioma over an intra-axial glioma. Context consistency: Consistent. The provided context indicates a 38-year-old female with “meningioma,” and imaging features align with this. Confidence: 90%.
3) Next best diagnostic step:
Further evaluation with post-contrast T1-weighted MRI sequences is recommended to confirm homogeneous strong enhancement and identify a dural tail or bone involvement. If MRI is already completed, correlation with pre- and post-contrast images supports surgical planning. Functional MRI or MR venography may be indicated if near eloquent brain areas or dural sinuses.
4) Key differential or confirmatory test:
Differential diagnoses include dural metastasis, hemangiopericytoma, and solitary fibrous tumor. Contrast-enhanced MRI with perfusion and diffusion-weighted imaging can help distinguish these entities (e.g., meningiomas typically enhance avidly and show slightly restricted diffusion). CT may help assess hyperostosis or calcification, often seen with meningiomas but rare in metastasis.
5) Possible treatment or management:
Surgical resection is the mainstay for symptomatic or large lesions. For incompletely resectable or recurrent lesions, adjunct radiotherapy (conformal or stereotactic radiosurgery) may be considered. Observation with serial imaging may be appropriate in incidental, small, asymptomatic cases. Postoperative follow-up MRI is essential to monitor for recurrence.
- A well-defined, extra-axial, dural-based mass is visible over the image-right (patient-left) frontoparietal convexity region.
- The lesion shows heterogeneously hyperintense signal intensity on this FLAIR MRI sequence.
- There is adjacent cortical sulcal effacement and underlying vasogenic edema extending into the adjacent white matter.
- Associated mild local mass effect with rightward (image-left, patient-right) midline shift is evident.
- The lesion margin appears broad-based against the inner table of the skull, with subtle dural thickening (“dural tail” sign possible).
- No hemorrhagic or cystic necrosis component clearly noted on this single sequence.
- Ventricles appear compressed on the image-right (patient-left) side due to mass effect.
- Cortical gray–white differentiation otherwise preserved outside the area of edema.
2) Most likely diagnosis and why:
Extra-axial dural-based mass consistent with meningioma. The smooth, broad-based extra-axial location, dural attachment, and presence of vasogenic edema with mass effect are characteristic features of a meningioma. The rounded contour and preservation of cortical gray–white matter interface favor a meningioma over an intra-axial glioma. Context consistency: Consistent. The provided context indicates a 38-year-old female with “meningioma,” and imaging features align with this. Confidence: 90%.
3) Next best diagnostic step:
Further evaluation with post-contrast T1-weighted MRI sequences is recommended to confirm homogeneous strong enhancement and identify a dural tail or bone involvement. If MRI is already completed, correlation with pre- and post-contrast images supports surgical planning. Functional MRI or MR venography may be indicated if near eloquent brain areas or dural sinuses.
4) Key differential or confirmatory test:
Differential diagnoses include dural metastasis, hemangiopericytoma, and solitary fibrous tumor. Contrast-enhanced MRI with perfusion and diffusion-weighted imaging can help distinguish these entities (e.g., meningiomas typically enhance avidly and show slightly restricted diffusion). CT may help assess hyperostosis or calcification, often seen with meningiomas but rare in metastasis.
5) Possible treatment or management:
Surgical resection is the mainstay for symptomatic or large lesions. For incompletely resectable or recurrent lesions, adjunct radiotherapy (conformal or stereotactic radiosurgery) may be considered. Observation with serial imaging may be appropriate in incidental, small, asymptomatic cases. Postoperative follow-up MRI is essential to monitor for recurrence.
📑 Guidelines Summary (uploaded diagnosis) — Meningioma
Imaging evaluation of suspected or known brain tumors focuses on diagnosis, presurgical planning, and treatment response assessment across diverse clinical settings.
- New neurologic deficit, seizure, or headache with suspicion of mass: MRI brain with and without contrast is first-line.
- CT head without contrast preferred for acute presentation or emergent assessment of hemorrhage or mass effect.
- Suspected metastatic disease: MRI brain with contrast for sensitivity to small lesions and posterior fossa evaluation.
- Unstable or contraindicated for MRI: contrast-enhanced CT brain as alternative.
- Postoperative or post-treatment surveillance: MRI brain with contrast at defined intervals for recurrence or progression.
- Pediatric or pregnant patients: avoid ionizing radiation; use MRI without contrast if safe.
- Non-contrast MRI sequences important for hemorrhagic, calcified, or postoperative changes when contrast cannot be given.
- Advanced techniques (MR perfusion, spectroscopy, diffusion) aid tumor grading and differentiation from radiation necrosis.
- Imaging not indicated for benign headache or neurologic symptoms clearly unrelated to intracranial disease.
- Follow-up interval imaging tailored to tumor type, treatment response, and symptom evolution.
- Pitfalls include mistaking treatment changes or infection for tumor progression; correlate with clinical and lab data.
🤖 Guidelines Summary (AI diagnosis) — Brain Tumors
Guidelines Summary of AI Suggestion diagnosis is the same as the uploaded diagnosis. Please read above.
Comments
No comments yet.
Please log in to comment