Low grade diffuse astrocytoma
Low confidence
High confidence
- Age: 38
- Sex: Female
- Modality: MRI
- Region: Brain
- Country: N/A
- State: N/A
- City: N/A
- Diagnosis: Low grade (WHO Gr2) diffuse astrocytoma
🧠 AI Suggestion
1) Findings:
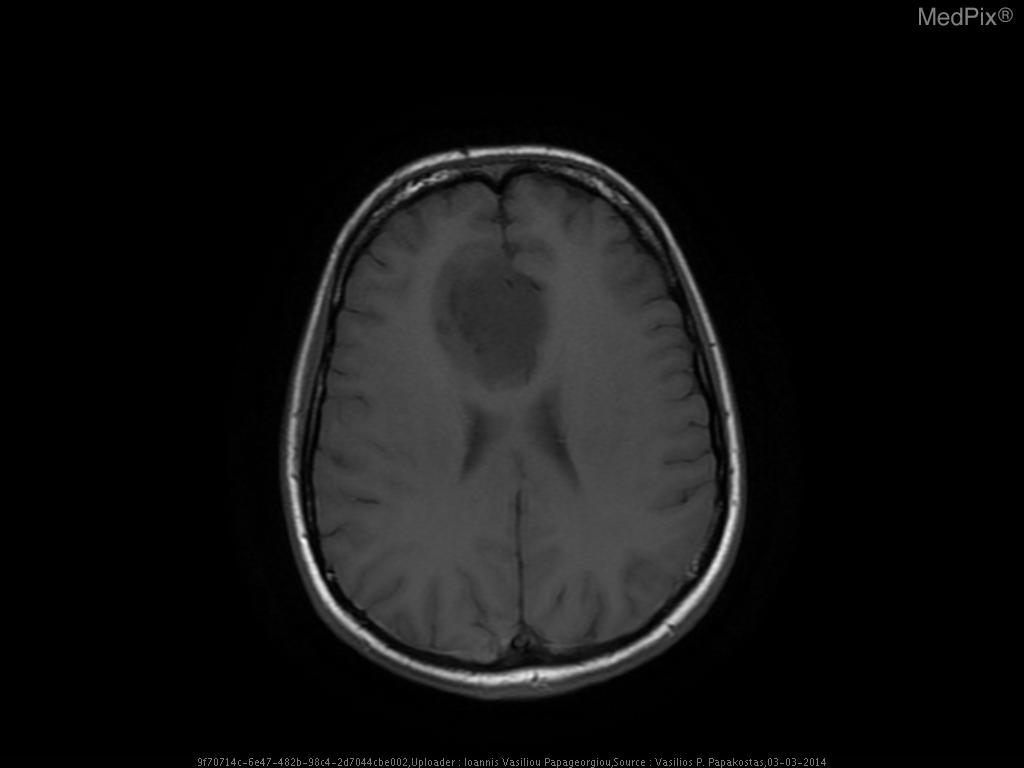
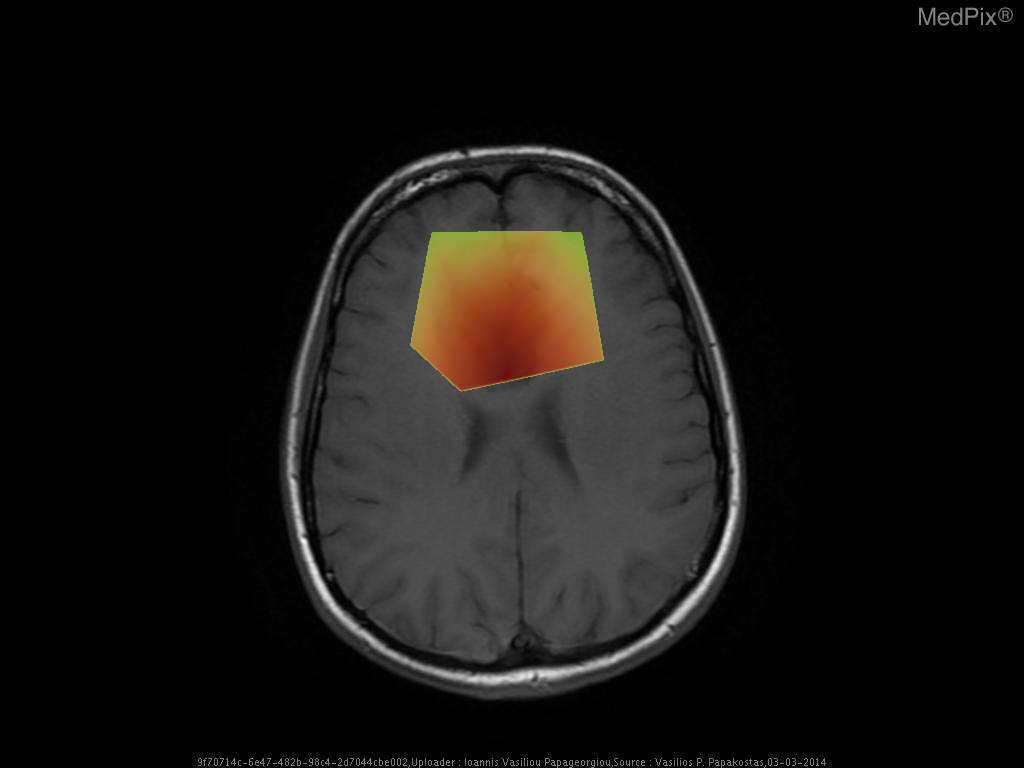
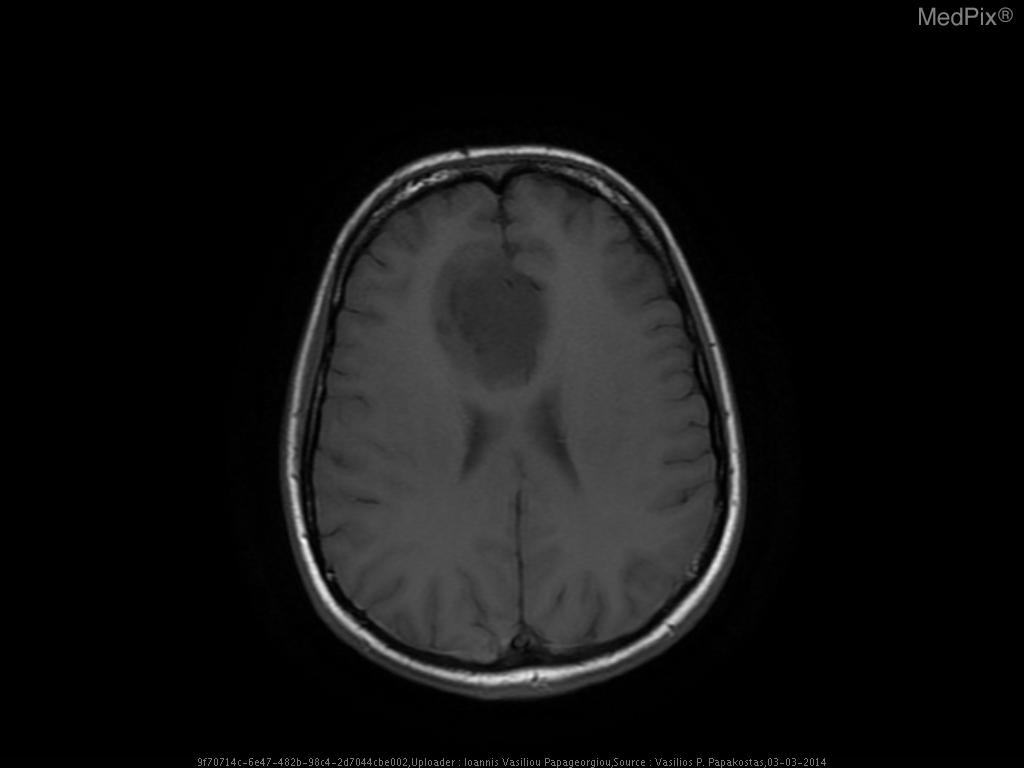
- Axial T1-weighted MRI brain shows a poorly defined, expansile lesion involving the image-right (patient-left) frontal lobe.
- The lesion demonstrates low T1 signal intensity relative to normal cortical gray matter.
- Minimal or no associated enhancement or hemorrhage visible on this non-contrast sequence.
- Mild mass effect evidenced by effacement of adjacent cortical sulci and mild displacement of the local midline toward image-left (patient-right).
- Gray-white differentiation appears blunted within the lesion region, suggesting infiltrative rather than circumscribed growth.
- No overt necrosis, cystic change, or intralesional hemorrhage visible on this slice.
- Surrounding brain parenchyma shows mild T1 hypointensity, potentially reflecting mild edema or infiltration.
- Ventricles appear slightly compressed on the image-right (patient-left) side, consistent with localized expansile mass effect.
2) Most likely diagnosis and why:
Low-grade diffuse astrocytoma (WHO Grade
2). This is favored because of the nonenhancing, poorly marginated, T1-hypointense and mildly expansile frontal lobe lesion without necrosis or hemorrhage—classic for a diffusely infiltrative glioma of low grade. Lack of enhancement or necrosis argues against high-grade glioma. Context consistency:
Consistent — the provided context aligns well with the imaging findings of a low-grade diffuse astrocytoma. Confidence: 90%.
3) Next best diagnostic step:
Thin-slice T2- and FLAIR-weighted MRI sequences should be reviewed to better delineate lesion extent and infiltration pattern. Contrast-enhanced T1-weighted imaging could confirm the absence of enhancement. Advanced MRI (MR spectroscopy, diffusion tensor imaging, perfusion) could further characterize metabolic and vascular features. Stereotactic biopsy would provide histopathologic confirmation.
4) Key differential or confirmatory test:
Differential includes oligodendroglioma, demyelinating pseudotumor, and cortical dysplasia. IDH mutation testing and 1p/19q codeletion analysis on biopsy are critical confirmatory markers distinguishing astrocytoma from oligodendroglioma. MR spectroscopy may demonstrate elevated choline and reduced NAA supporting a glioma.
5) Possible treatment or management:
Primary management involves maximal safe surgical resection to obtain tissue diagnosis and reduce tumor burden. Depending on pathology, adjuvant radiotherapy and/or chemotherapy (e.g., temozolomide) may be considered. Postoperative serial MRI monitoring is essential for detecting recurrence or malignant transformation. Multidisciplinary neuro-oncology follow-up is recommended.
- Axial T1-weighted MRI brain shows a poorly defined, expansile lesion involving the image-right (patient-left) frontal lobe.
- The lesion demonstrates low T1 signal intensity relative to normal cortical gray matter.
- Minimal or no associated enhancement or hemorrhage visible on this non-contrast sequence.
- Mild mass effect evidenced by effacement of adjacent cortical sulci and mild displacement of the local midline toward image-left (patient-right).
- Gray-white differentiation appears blunted within the lesion region, suggesting infiltrative rather than circumscribed growth.
- No overt necrosis, cystic change, or intralesional hemorrhage visible on this slice.
- Surrounding brain parenchyma shows mild T1 hypointensity, potentially reflecting mild edema or infiltration.
- Ventricles appear slightly compressed on the image-right (patient-left) side, consistent with localized expansile mass effect.
2) Most likely diagnosis and why:
Low-grade diffuse astrocytoma (WHO Grade
2). This is favored because of the nonenhancing, poorly marginated, T1-hypointense and mildly expansile frontal lobe lesion without necrosis or hemorrhage—classic for a diffusely infiltrative glioma of low grade. Lack of enhancement or necrosis argues against high-grade glioma. Context consistency:
Consistent — the provided context aligns well with the imaging findings of a low-grade diffuse astrocytoma. Confidence: 90%.
3) Next best diagnostic step:
Thin-slice T2- and FLAIR-weighted MRI sequences should be reviewed to better delineate lesion extent and infiltration pattern. Contrast-enhanced T1-weighted imaging could confirm the absence of enhancement. Advanced MRI (MR spectroscopy, diffusion tensor imaging, perfusion) could further characterize metabolic and vascular features. Stereotactic biopsy would provide histopathologic confirmation.
4) Key differential or confirmatory test:
Differential includes oligodendroglioma, demyelinating pseudotumor, and cortical dysplasia. IDH mutation testing and 1p/19q codeletion analysis on biopsy are critical confirmatory markers distinguishing astrocytoma from oligodendroglioma. MR spectroscopy may demonstrate elevated choline and reduced NAA supporting a glioma.
5) Possible treatment or management:
Primary management involves maximal safe surgical resection to obtain tissue diagnosis and reduce tumor burden. Depending on pathology, adjuvant radiotherapy and/or chemotherapy (e.g., temozolomide) may be considered. Postoperative serial MRI monitoring is essential for detecting recurrence or malignant transformation. Multidisciplinary neuro-oncology follow-up is recommended.
📑 Guidelines Summary (uploaded diagnosis) — Low grade (WHO Gr2) diffuse astrocytoma
Appropriate imaging for suspected or known brain tumors depends on presentation, tumor type, and need for surgical or radiotherapy planning.
- New focal neurologic deficit or seizure warrants MRI brain with and without contrast as first-line imaging.
- Noncontrast CT is preferred for initial triage of acute deterioration or hemorrhagic presentation before MRI.
- Contrast-enhanced MRI best delineates tumor margins, edema, and relationship to eloquent cortex or vessels.
- MRI with perfusion and spectroscopy adds value for grading and differentiating tumor from treatment change.
- CT or MRI before biopsy or resection guides surgical approach and assesses mass effect or herniation risk.
- Routine imaging not indicated for nonspecific headache without neurologic findings or seizure history.
- In patients with contraindications to MRI, contrast-enhanced CT offers limited but acceptable tumor evaluation.
- MRI is preferred for follow-up after surgery, radiation, or chemotherapy to monitor recurrence or response.
- Red flags such as new seizures, papilledema, or cognitive decline justify urgent imaging.
- Beware pitfalls—enhancement may represent post-treatment effect, radiation necrosis, or infection rather than true progression.
- Advanced imaging (DTI, fMRI) assists presurgical mapping of motor and language areas when tumor proximity is suspected.
🤖 Guidelines Summary (AI diagnosis) — Brain Tumors
Guidelines Summary of AI Suggestion diagnosis is the same as the uploaded diagnosis. Please read above.
Comments
No comments yet.
Please log in to comment