Swimming-Induced Pulmonary Edema (SIPE)


Low confidence
High confidence
- Age: 26
- Sex: Male
- Modality: X-ray
- Region: Chest
- Country: N/A
- State: N/A
- City: N/A
- Diagnosis: Swimming-Induced Pulmonary Edema (SIPE)
🧠 AI Suggestion
1) Findings:
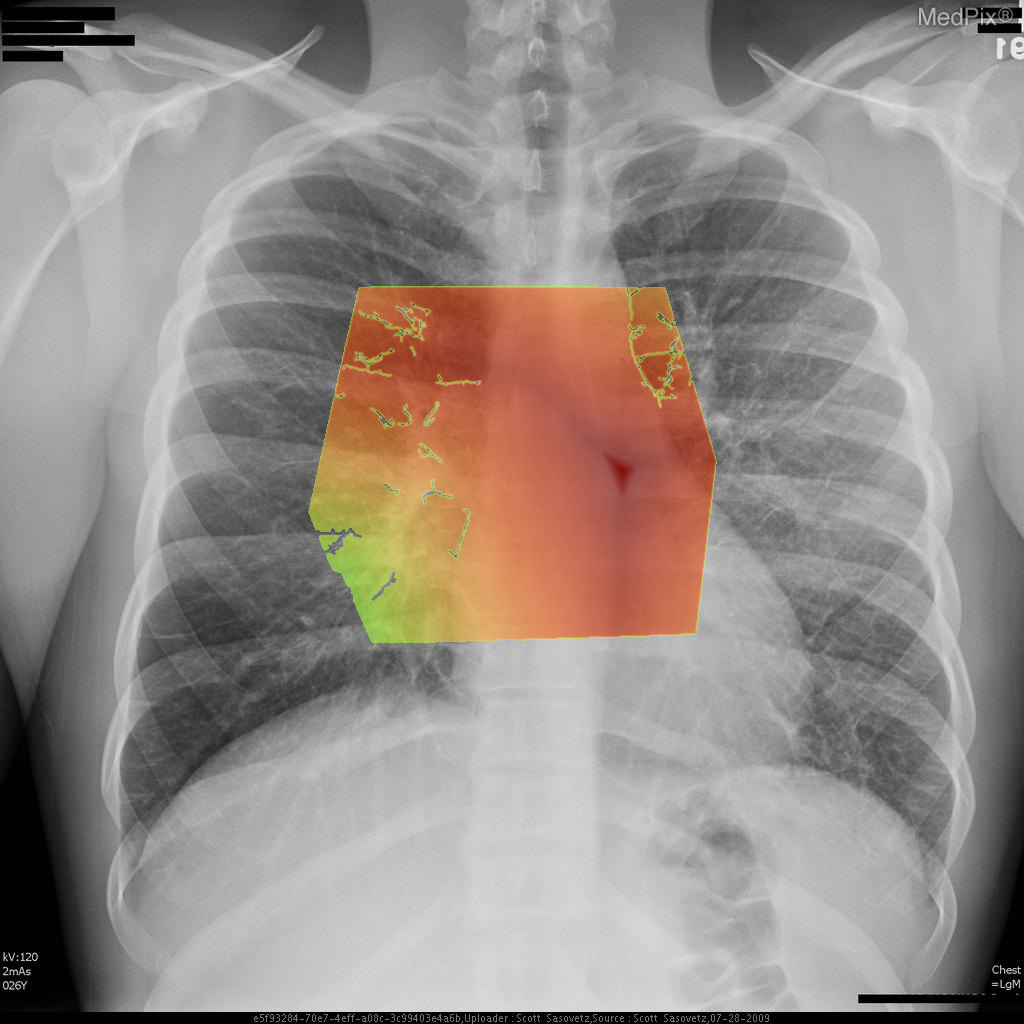
- Adequate inspiratory chest X-ray with clear visualization of both lungs, mediastinum, and diaphragm.
- Cardiac silhouette is normal in size; cardiac apex lies image-right (patient-left), consistent with expected anatomy.
- Pulmonary vasculature appears mildly prominent centrally, with increased perihilar markings suggestive of vascular congestion.
- Subtle hazy ground-glass type opacities noted in the perihilar regions, extending outward in a symmetric pattern (more conspicuous centrally than at the periphery).
- No focal lobar consolidation, no pleural effusion, and no pneumothorax identified.
- Costophrenic angles appear sharp bilaterally.
- Bony thorax visualized without acute abnormality.
2) Most likely diagnosis and why:
Findings are most consistent with pulmonary edema. The hazy bilateral perihilar opacities and vascular congestion suggest an interstitial/alveolar fluid process consistent with pulmonary edema rather than focal pneumonia or chronic interstitial disease. The absence of cardiomegaly makes non-cardiogenic causes more likely (such as swimming-induced pulmonary edema). Context consistency: Consistent — the described clinical context (young swimmer with acute onset) aligns well with non-cardiogenic pulmonary edema findings. Confidence: 80%.
3) Next best diagnostic step:
A confirmatory and more sensitive imaging test would be chest CT to exclude alternative causes of interstitial/alveolar infiltrates and better evaluate for edema distribution. Bedside lung ultrasound could also demonstrate B-lines supporting alveolar-interstitial edema. Concurrently, clinical correlation with oxygen saturation and symptoms is critical.
4) Key differential or confirmatory test:
Differentials include viral/atypical pneumonia, aspiration, and other causes of acute lung injury. A confirmatory test would be echocardiography to exclude cardiogenic causes if history or exam suggests cardiac dysfunction. Measurement of BNP can also help differentiate cardiogenic from non-cardiogenic pulmonary edema.
5) Possible treatment or management:
Management focuses on supportive therapy: oxygen supplementation, careful monitoring, and cessation of strenuous activity/swimming. In SIPE, symptoms usually resolve quickly with rest and oxygen. If severe respiratory distress occurs, noninvasive ventilation or intubation may be required. Long-term, patients may benefit from counseling about SIPE recurrence risk and strategies for prevention during swimming or diving activities
- Adequate inspiratory chest X-ray with clear visualization of both lungs, mediastinum, and diaphragm.
- Cardiac silhouette is normal in size; cardiac apex lies image-right (patient-left), consistent with expected anatomy.
- Pulmonary vasculature appears mildly prominent centrally, with increased perihilar markings suggestive of vascular congestion.
- Subtle hazy ground-glass type opacities noted in the perihilar regions, extending outward in a symmetric pattern (more conspicuous centrally than at the periphery).
- No focal lobar consolidation, no pleural effusion, and no pneumothorax identified.
- Costophrenic angles appear sharp bilaterally.
- Bony thorax visualized without acute abnormality.
2) Most likely diagnosis and why:
Findings are most consistent with pulmonary edema. The hazy bilateral perihilar opacities and vascular congestion suggest an interstitial/alveolar fluid process consistent with pulmonary edema rather than focal pneumonia or chronic interstitial disease. The absence of cardiomegaly makes non-cardiogenic causes more likely (such as swimming-induced pulmonary edema). Context consistency: Consistent — the described clinical context (young swimmer with acute onset) aligns well with non-cardiogenic pulmonary edema findings. Confidence: 80%.
3) Next best diagnostic step:
A confirmatory and more sensitive imaging test would be chest CT to exclude alternative causes of interstitial/alveolar infiltrates and better evaluate for edema distribution. Bedside lung ultrasound could also demonstrate B-lines supporting alveolar-interstitial edema. Concurrently, clinical correlation with oxygen saturation and symptoms is critical.
4) Key differential or confirmatory test:
Differentials include viral/atypical pneumonia, aspiration, and other causes of acute lung injury. A confirmatory test would be echocardiography to exclude cardiogenic causes if history or exam suggests cardiac dysfunction. Measurement of BNP can also help differentiate cardiogenic from non-cardiogenic pulmonary edema.
5) Possible treatment or management:
Management focuses on supportive therapy: oxygen supplementation, careful monitoring, and cessation of strenuous activity/swimming. In SIPE, symptoms usually resolve quickly with rest and oxygen. If severe respiratory distress occurs, noninvasive ventilation or intubation may be required. Long-term, patients may benefit from counseling about SIPE recurrence risk and strategies for prevention during swimming or diving activities
📑 Guidelines Summary (uploaded diagnosis) — Swimming-Induced Pulmonary Edema (SIPE)
Imaging choices for pleural effusion or pleural disease depend on acuity, suspected cause, and presence of concerning clinical features.
- Chest radiograph is first-line for newly suspected pleural effusion or pleural abnormality.
- Ultrasound is preferred for guiding thoracentesis or distinguishing effusion from pleural thickening.
- CT chest without contrast helps characterize pleural fluid, masses, or calcification when malignancy or chronic disease is suspected.
- Contrast-enhanced CT can evaluate pleural enhancement, nodularity, or suspected empyema and malignancy.
- Do not routinely image small, stable, clearly transudative effusions without concerning features.
- MRI chest is useful when CT findings are equivocal for pleural tumor, invasion, or chest wall involvement.
- Consider CT pulmonary angiography if concurrent pulmonary embolism is suspected causing effusion.
- Reimage with CT after treatment if effusion persists or atypical features raise concern for underlying malignancy.
- Red flags: loculated effusion, hemothorax, rapid reaccumulation, or pleural nodularity signal need for advanced imaging.
- Pitfalls include mistaking subpulmonic effusion for elevated diaphragm or missing effusion on supine x-ray.
🤖 Guidelines Summary (AI diagnosis) — Workup of Pleural Effusion or Pleural Disease
Guidelines Summary of AI Suggestion diagnosis is the same as the uploaded diagnosis. Please read above.
Comments
No comments yet.
Please log in to comment