Pneumonia XR
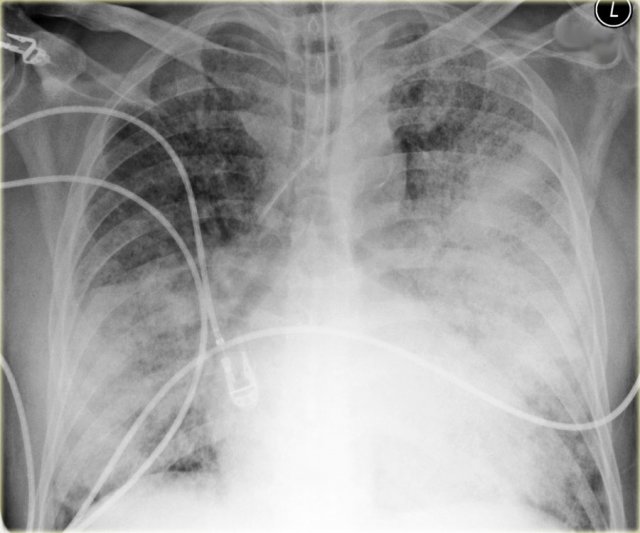
- Age: 87
- Sex: Male
- Modality: X-ray
- Region: Chest
- Country: N/A
- State: N/A
- City: N/A
- Diagnosis: Pneumonia
🧠 AI Suggestion
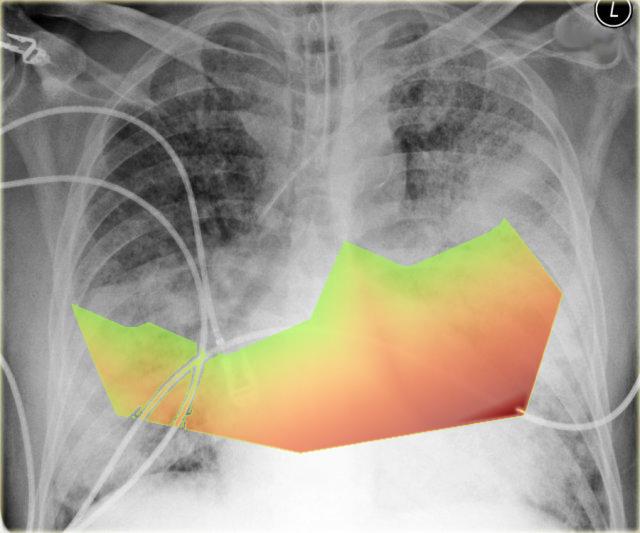
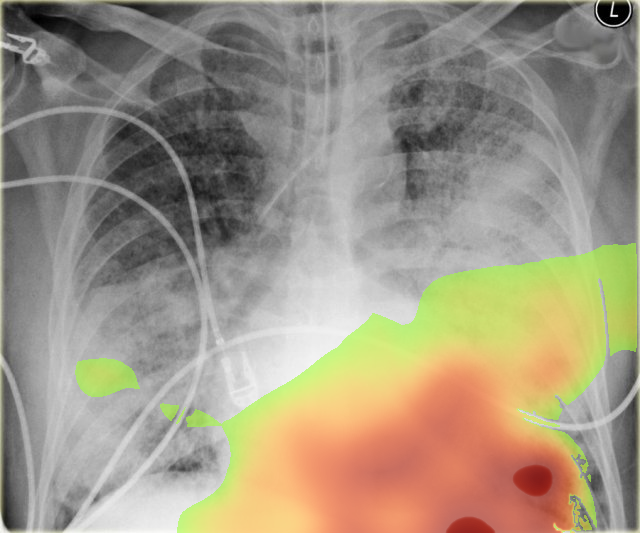
- Diffuse, bilateral airspace opacities involving both image-right (patient-left) and image-left (patient-right) lungs, confluent in the lower zones, consistent with alveolar filling.
- Relative sparing of apices but diffuse ground-glass and consolidation throughout mid-to-lower zones.
- No large pleural effusion or pneumothorax detected; costophrenic angles partially obscured by consolidation.
- Cardiothoracic ratio appears at the upper limit of normal but difficult to fully assess due to diffuse opacities.
- Endotracheal tube is present, tip positioned above the carina.
- Other support devices noted: cardiac pacemaker lead projecting over the image-left (patient-right) chest.
- Pulmonary vascular markings are indistinct, suggesting interstitial edema component.
- No obvious rib fracture or bony abnormality is identified.
2) Most likely diagnosis and why:
The most likely diagnosis is acute respiratory distress syndrome (ARDS) or severe pulmonary edema. The diffuse bilateral alveolar infiltrates without clear focal consolidation pattern, presence of endotracheal intubation, and indistinct vascular margins raise suspicion. Cardiomegaly is not prominent, which argues slightly against isolated cardiogenic pulmonary edema, making ARDS from sepsis, aspiration, or severe infection more likely.
3) Next best diagnostic step:
The next best step would be correlation with arterial blood gases to assess severity of hypoxemia and determine the PaO₂/FiO₂ ratio for ARDS classification. Evaluating fluid status with urine output, hemodynamics, and possibly echocardiography would also help differentiate non-cardiogenic versus cardiogenic pulmonary edema.
4) Key differential or confirmatory test:
Key differentials include cardiogenic pulmonary edema, multifocal pneumonia, and diffuse alveolar hemorrhage. Confirmatory or distinguishing tests include echocardiography for left ventricular function and filling pressures, bronchoalveolar lavage (if indicated) to exclude hemorrhage or infection, and BNP levels to evaluate for cardiac contribution.
5) Possible treatment or management:
Management involves lung-protective ventilation (low tidal volume, plateau pressure <30 cmH₂O) if ARDS is confirmed, along with optimizing oxygenation using PEEP titration. Fluid balance should be carefully managed, with conservative fluid strategies shown to improve outcomes in ARDS. In severe refractory hypoxemia (PaO₂/FiO₂ <80 despite optimal settings), rescue therapies such as prone positioning or ECMO may be considered in tertiary centers. Concurrent treatment of the underlying cause (e.g., antibiotics for sepsis, diuretics for cardiac failure) is necessary
📑 Guidelines Summary (uploaded diagnosis) — Pneumonia
Imaging for acute respiratory illness in immunocompetent patients depends on severity, red flags, suspected complications, and response to therapy.
- No imaging for mild acute bronchitis without comorbidities or hypoxemia.
- Chest radiograph first-line for suspected pneumonia, unexplained fever, or abnormal lung exam.
- Chest radiograph indicated in hypoxemia, leukocytosis, tachypnea, or elderly with nonspecific symptoms.
- CT chest without IV contrast if chest radiograph equivocal or complications suspected.
- CT indicated for suspected abscess, empyema, or cavitary lesion not explained by radiograph.
- High-resolution CT for recurrent or nonresolving pneumonia despite treatment.
- No role for immediate CT in typical mild viral upper respiratory illness.
- Chest radiograph helps exclude alternative diagnoses such as heart failure or malignancy.
- CT pulmonary angiography for acute respiratory illness with suspicion of pulmonary embolism.
- Portable chest radiograph acceptable in unstable or critically ill patients.
- Follow-up imaging after pneumonia only if persistent symptoms or high-risk for malignancy.
🤖 Guidelines Summary (AI diagnosis) — Workup of Pleural Effusion or Pleural Disease
Imaging evaluation of pleural effusion or pleural disease guides diagnosis, identifies causes, and directs safe intervention strategies.
- Chest radiography is first-line for new pleural effusion or suspected pleural disease.
- Ultrasound is preferred for bedside detection and guidance of thoracentesis.
- CT chest with contrast clarifies pleural thickening, loculation, or suspected mass after inconclusive radiograph or ultrasound.
- Non-contrast CT may suffice when IV contrast is contraindicated, though subtle enhancement patterns may be missed.
- MRI or MR angiography can assess pleural tumors or chest wall invasion when CT is limited.
- Do not routinely image simple, stable, transudative effusions responding to therapy.
- Urgent CT or ultrasound is warranted with fever, trauma, or suspicion of empyema.
- Image-guided sampling recommended for atypical, recurrent, or unilateral exudative effusions.
- Short-term follow-up radiography verifies resolution after drainage or treatment of pneumonia-associated effusion.
- Pitfalls include mistaking pleural thickening for mass or overlooking small loculations without ultrasound guidance.
Comments
No comments yet.
Please log in to comment